|
Annual Wellness Visits have been linked to the improvement of the health of our senior beneficiaries and lowering their overall health costs. Tools and evidence-based strategies have been developed to facilitate our Accountable Care Organizations in the implementation and improvement of compliance with Annual Wellness Visits. Key strategies for success have been identified to aid your ACO in increasing Annual Wellness Visit compliance rates. The following four primary strategies are supported by this toolkit: • Make AWV an ACO priority by identifying AWV champions • Promote patient engagement with scripting, reminder letters/cards, proactive scheduling practices and patient facing public reminders • Optimize clinic management of AWV by top down communication of AWV as a priority, increasing the visibility of the data, utilizing pursuit lists to identify patients needing an AWV and increasing the use of telehealth where feasible • Enhance the workflow efficiencies of an AWV through use of a multidisciplinary team approach and incorporating the use of allied professionals, telehealth visits and optimizing EHR documentation |

For Providers
Your partner in the transition to value-based payments from traditional fee for service
Fee for service payment models for health care in the United States have grown unsustainable. While the United States economy spends >18% on health care (three times more than other countries), it does not exhibit better outcomes. Analysis of health care costs determined that of total health care spending, 30% has been identified as unnecessary, ineffective, overpriced and wasteful.
In order to transform how health care providers are reimbursed for services rendered, the Centers for Medicare & Medicaid Services (CMS) introduced an array of value-based care models. Private payers have in turn adopted similar models of accountable, value-based care.
Goal of Value-Based Payments
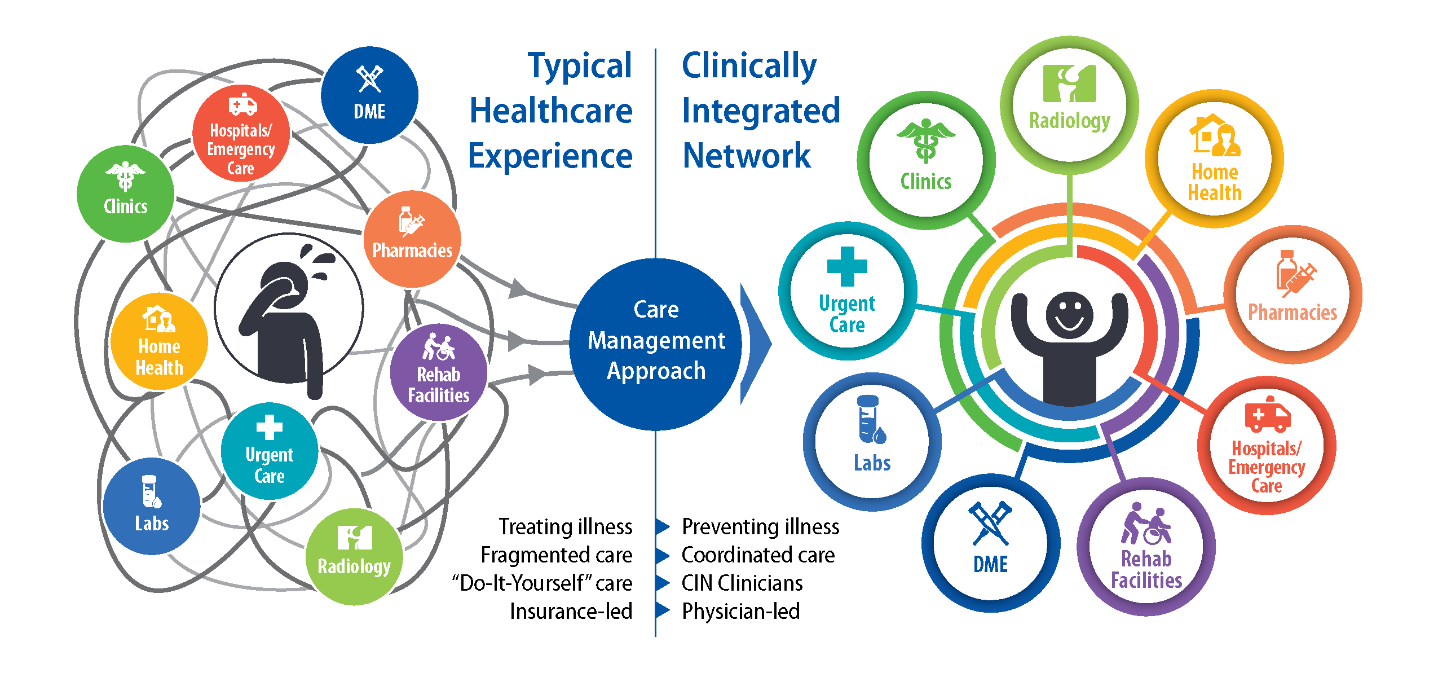
Replace fragmented, fee-for-service care with comprehensive, coordinated care using payment models that hold organizations accountable for cost control and quality gains. By advancing the triple aim of:
- Providing comprehensive and coordinated care for individuals
- Improving population health management strategies
- Reducing health care costs
“I believe that the culture of treating illness and emphasizing volume is slowly shifting to encouraging wellness and valuing quality. Annual wellness exams are a necessary part of that paradigm shift. People are living longer and healthier lives, and the focus on wellness is a change that is hopefully here to stay.”
– Thomas Coburn, MD CHI Saint Joseph Health Primary Care
Quality Reporting Resources
Driven By Data
Value-Based care is driven by data. In many cases it is not the quality of the care that needs improvement, it’s documentation of that quality care.
When patients receive more coordinated, appropriate, and effective care, providers are rewarded.
Our innovative care management strategy centers on the primary care component of health care. It is critical that primary care providers are connected seamlessly with all network providers, each with access to the tools and resources they need to provide the right care, at the right time, in the right place.
We use the most sophisticated and secure technology to:
- Monitor & report quality measures
- Produce patient-specific reports including open gaps in preventive care and risk stratification
- Access to data allowing you to make information-powered clinical decisions and reduce duplicative services
CHI Saint Joseph Health Partners monitors six different third-party payor shared savings/quality measure performance contracts, totaling 48 separate quality measures. Measures include preventative care screenings, immunizations, and completion of annual well visits as well as medications prescribed and monitored. Click on the tabs below to learn more about quality reporting resources.
As the seventh leading cause of death in the U.S., diabetes kills approximately 79,500 people a year. People with diabetes are at increased risk of serious health complications including vision loss, heart disease, stroke, kidney failure, amputation of toes, feet or legs, and premature death.
Improving diabetes management will require an expanded effort and improved focus from ambulatory leaders, providers and clinic staff across CommonSpirit Health. This toolkit has been developed to support implementation of evidenced-based best practices to address challenges in diabetes management within the clinic setting.
This resource advances efforts in diabetes care with a focus on the following areas for improvement:
1. Establish Diabetes Management as a Practice Priority
2. Optimize Diabetes Management Practices
3. Improve Diabetes Screening, Diagnosis and Monitoring
4. Engage & Support Patients in Self-Management of Diabetes
Improving depression screening and management will require an expanded effort and improved focus from ambulatory leaders, providers and clinic staff across CommonSpirit Health. This toolkit has been developed to support implementation of evidence-based best practices to address challenges in depression screening and management within the clinic setting.
This resource advances efforts in depression screening and management with a focus on the following areas for improvement:
1. Establish Depression Screening Management as Practice Priority
2. Optimize Workflow to Support Depression Screening & Follow Up
3. Engage and Support Patients in Self-Management of Depression
4. Establish a Defined Workflow for Provider Interpretation and Follow Up for Positive Screening Results
5. Deploy Evidence-Based Approach to Diagnosis, Treatment and Ongoing Management of Mild to Moderate Depression
Improve Medication Adherence with these tips:
Consider converting the patient’s prescription to a 90-day supply (when available).
This reduces the barrier of frequent travel to the pharmacy. (tip: Set your electronic medical record default to a 90-day supply.)
Review your patient list for patients that you consider high risk for non-adherence or develop a questionnaire to help understand patients’ adherence and potential barriers. Our clinical pharmacist can work with your patients to reduce additional barriers preventing them from maintain their prescribed regimen.
- Send to a home delivery or mail order pharmacy, further reducing the burden of travel.
- Prescribe a year’s supply of prescriptions at each annual visit to prevent refill gaps.
- If your patient is overdue for follow-up, send a one-time 30-day refill and immediately contact patient to schedule a visit.
- Schedule appointment with patient within the first seven days of discharge from an inpatient setting (or as soon as you are aware of discharge) to complete a medication reconciliation.
- Educate patients on how and when to take their medications and explain why this medication is important and potential adverse effects. Suggest pairing medications with a routine activity, use of a pillbox, or setting an alarm.
- Educate on “silent symptoms” and long-term compilations of diagnosis.
- Screen for depression as a potential contributor for not taking medications.
- Develop protocols or questionnaires to help understand potential adherence barriers.
- Recommend opt-in to pharmacy auto-refill and reminder calls.
- Prescribe generics to reduce cost barriers. Many are available with a $0 copay.
- Encourage members to review their plan or contact their insurer’s Member Services.
- When adjusting medications, issue a new prescription to ensure directions reflect the change.
- Ask patient to bring all medication to each visit.
- Discontinue unnecessary medications and consider lower doses.
- Consider once daily dosing or combination products when appropriate.
Reducing preventable and unplanned hospital readmissions is a national priority for payers, providers, and policymakers seeking to improve health care and lower costs. Tools and evidence-based strategies have been developed to facilitate facility implementation of our 7 day readmission reduction strategies.
7 Day Readmission Reduction Strategies for Success
• Identify high risk patients for readmission – establishing a mechanism to identify patients at high risk for readmission allows for the matching of the intensity of the discharge planning process to the risk of readmission.
• Match intensity of discharge planning to risk of readmission – ensure Multidisciplinary Rounds (MDRs) are completed on patients following a high risk patient admission as determined by the DRG or readmission risk score.
• Refer patients to the most appropriate post-acute setting – focus on the discharge disposition with the least restrictive setting needed to prevent readmission.
• Provide comprehensive patient discharge education – providing individualized patient and family discharge education is pivotal to improving patient outcomes, elevating healthcare quality and reducing unplanned readmissions.
• Promote cross-continuum communication – when hospitals, post-acute providers, home care agencies, patients and families work together to ensure patients are engaged in their care, follow treatment plans and get help before chronic conditions take a turn for the worse, better long-term health outcomes can be achieved for patients while limiting unplanned trips to the acute setting.
• Establish a multidisciplinary facility Readmission Committee – engaging in a monthly multidisciplinary readmission meeting, focusing on developing process improvement strategies and utilizing data to drive initiatives is a key strategy to reduce readmissions.
Please use these strategies and tools to implement these identified evidence-based strategies.
Improving hypertension management will require an expanded effort and improved focus from ambulatory leaders, providers and clinic staff across CommonSpirit Health. This toolkit has been developed to support implementation of evidenced-based, best practices to address challenges in hypertension management within the clinic setting.
Please use this resource and deploy referenced tools to advance efforts in hypertension care, with a focus on the following areas for improvement:
1. Establish hypertension improvement as a practice priority
2. Ensure a process exists to support accurate blood pressure measurement
3. Support patients in self-management of

.pdf/_jcr_content/renditions/cq5dam.web.1440.405.jpeg)
.pdf/_jcr_content/renditions/cq5dam.web.1440.405.jpeg)